Nephrology
Hemodialysis: All You Need To Know
Hemodialysis: All You Need To Know Dec 11, 2020
 Hemodialysis: All you need to know
Hemodialysis is a treatment for filtering waste and water from your blood, as your kidneys did when they were healthy. Hemodialysis helps to control important minerals such as potassium, sodium, and calcium in your blood and control blood pressure.
Hemodialysis can help you feel better and live longer, but it is not a treatment for kidney failure.
What happens during hemodialysis?
During hemodialysis, your blood goes through a filter, which is called a dialyzer outside your body. The dialyzer is sometimes called the "artificial kidney".
At the beginning of a hemodialysis treatment, a dialysis nurse or technician places two needles in your hand. Numb cream or spray may be used if the needle irritates you. Each needle is attached to a soft tube connected to a dialysis machine.
During hemodialysis, your blood is pumped through a filter, called a dialyzer.
The dialysis machine pumps blood through the filter and brings blood back to your body. During the procedure, the dialysis machine checks your blood pressure and controls how quickly
* Blood flows through the filter
* Fluids are released from your body
What happens to my blood when in the filter?
Blood enters one end of the filter and is forced into several, very thin, hollow fibers. As your blood passes through the hollow fibers, the dialysis solution passes in the opposite direction to the outside of the fibers. Waste products from your blood move to the dialysis solution. The filtered blood stays in hollow fibers and returns to your body.
In the filter, your blood flows inside hollow fibers that filter waste and excess salt and water.
Your nephrologist - a doctor specializing in kidney problems - will prescribe a dialysis prescription to meet your needs. The dialysis solution contains water and chemicals that are added to safely remove waste, excess salt, and fluid from your blood. Your doctor may adjust the balance of the chemicals in the solution if
* Your blood test shows that you have few or very few minerals in your blood, such as potassium or calcium
* You have problems like low blood pressure or muscle cramps during dialysis
Has the dialyzer done everything to get my kidneys at once?
No, hemodialysis can change part of your kidney function, but not all. Dialysis will help improve your energy level, and the changes you make to your diet can help you feel better. Limiting how much water and other fluids you drink through foods can help keep too much fluid from building up in your body between treatments. Medications during dialysis help you in maintaining your health.
Where can I get hemodialysis?
You can get treatment at a dialysis center or at home. Every place has its pros and cons.
Dialysis center
Most people go to a dialysis center for treatment. At the dialysis center, health care professionals are set up and help you connect with the dialysis machine. A team of health care workers will be available to assist you. You will continue to see your doctor. Other members of the team may include nurses, health care technicians, a dietitian and a social worker.
Set schedule
You will have a fixed time slot for your treatment, usually three times per week: Monday, Wednesday, and Friday; Or Tuesday, Thursday and Saturday. Each dialysis session lasts approximately 4 hours. When choosing a dialysis schedule, think about your work and child care or other caregiver duties.
Night option
Some dialysis centers offer nocturnal treatment. These treatments take place at a dialysis center 3 nights a week at bedtime, which takes longer. Now overnight dialysis treatment means
* Your days are free.
* You have less dietary changes.
* Your liquid allowance (how much liquid you can drink) is close to normal.
* You may have a better quality of life than the standard hemodialysis schedule. Long treatment sessions can ease your symptoms.
How can I get a dialysis center?
Seek the help of your doctor. Most major cities have more than one dialysis center to choose from. You can visit the centers to see which one of your requirements is most suitable. For example, you can ask about the use of laptops and cellphones as well as the rules of a center for visitors. You want the center to be close to your home to save travel time. If you live in a rural area, the nearest dialysis center may be away from your home. If you have a hard time coming to a dialysis center, you may want to consider home dialysis treatments such as home hemodialysis or peritoneal dialysis.
Home hemodialysis
Home hemodialysis allows you longer or more frequent dialysis, as do healthy kidneys - usually three to seven times per week, and with treatment sessions that last 2 to 10 hours. Machines for home use are small enough to sit on an end table.
If you want to do your treatment at home, you still consult your doctor once per month.
Flexible schedule
You can choose a schedule that fits your way of living. you can use
* Normal household hemodialysis - 3 to 5 hours three times a week or every other day
* Short daily hemodialysis - 5 to 7 days per week for 2 to 4 hours at a time
* Perform hemodialysis at night - three to six times per week at bedtime
Your doctor will decide how many treatments you need each week for daily or nightly home hemodialysis.
More dialysis filters your blood more thoroughly
Compared with a normal hemodialysis, daily or overnight household hemodialysis will give you
* Eat and drink more commonly
* Take low blood pressure medications
Healthy kidneys work 24 hours, 7 days a week. Getting more hemodialysis has the benefits of having a healthy kidney and lessens your chances for problems with a normal hemodialysis, such as
* Cramps by quickly removing too much fluid in painful muscles
* High blood pressure, which can cause a headache or, in rare cases, a stroke
* Low blood pressure, which can make you unconscious, make you feel sick in your stomach, or more likely to fall
* High phosphate levels, which can weaken bones and itch your skin
Better quality of life
You may feel tired for several hours after each treatment with normal hemodialysis. Those who have switched from normal hemodialysis to longer or persistent hemodialysis report feeling better with more energy, less nausea, and better sleep. They can also report better quality of life
How do I prepare for hemodialysis?
Dialysis is a complex treatment that takes time to understand. Because most people do not feel ill until shortly before starting dialysis, you will still feel good when your doctor talks to you about getting ready for dialysis. No one wants to get you started on dialysis before you need it, but preparing for dialysis takes time.
Take care of the blood vessels in your arms
It is important for you to protect your hand veins before starting dialysis. If you have kidney disease, health care providers should remind them to pour blood into the veins below your wrist and only IV lines; For example, ask them to use a vein on the back of their hand. If the vein of one arm is damaged by the IV line or by repeated blood drawing, it may not be used for vein dialysis.
Vascular Access Surgery
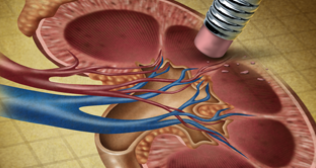
An important step before starting hemodialysis treatment is minor surgery to create vascular access. Your vascular access will be your lifeline, through which you will connect with the dialer. Dialysis transfers blood through the filter at a high rate. Blood flow is very strong. The machine extracts and returns about one point of blood from your body every minute. The access will be the place on your body where you insert needles to allow your blood to flow and return to your body at a high rate of dialysis by needle.
Three types of vascular access exist
* AV Fischula
* AV graft
* A catheter
Work closely with your nephrologist and vascular surgeon - a surgeon who works with blood vessels - to ensure that the vascular access is ready for use when you are ready for dialysis.
The surgeon connects a vein to a vein to make an AV fistula.
Avi fistula
The best type of long-term access is an AV facula. To make an AV fistula, a surgeon usually connects a vein to your hand. An artery is a blood vessel that carries blood away from your heart. A vein is a blood vessel that carries blood to your heart. When the surgeon connects an artery to a vein, the vein becomes wider and thicker, making it easier for the needles to give space for dialysis. The AV fistula also has a larger diameter that allows your blood to drain out and return quickly to your body. The goal is to allow high blood flow so that the greatest amount of blood can pass through the dialyzer.
The AV fistula is a blood vessel that is widened and strengthened by surgeons with needles that allow blood to exit and return to the dialysis machine.
AV fistula is considered the best option because it
* Provides the highest blood flow for dialysis
* Less likely to become infected or clot
* lasts longer
Most people can go home after outpatient surgery. And most operations are performed in local anesthesia.
AV grafts
If problems with your veins prevent you from having an AV fistula, you may need an AV graft instead. To make AV grafts, your surgeon uses a man-made tube to connect an artery to a vein. You can use AV grafts for dialysis immediately after surgery. However, you are more likely to have infections and blood clotting problems. Repeated blood clots can stop the flow of blood through the graft and make dialysis difficult or impossible.
Catheter for temporary access
If your kidney disease has progressed quickly, or you have not had vascular access before needing dialysis, you may need a venous catheter - a small, soft tube called a vein in your neck, chest, or leg. Is inserted in As temporary access. A nephrologist or an interventional radiologist - a doctor who uses medical imaging devices to perform the surgery - implants Venous catheters when you are in a hospital or in an outpatient clinic. You will receive local anesthesia and medication to keep you calm and relaxed during the procedure.
What changes do I need to make when I start hemodialysis?
You have to adjust your life to include your dialysis treatment sessions in your routine. If you have in-center dialysis, you may need to rest after each treatment. Adjusting for the effects of kidney failure and the time you spend on dialysis can be difficult. You may need to make changes in your work or home life by abandoning certain activities and responsibilities. It can be difficult for you and your family to accept these changes.
You have to change what you eat and drink. Your health care team can adjust the medicines you take.
Take care of your access
Your access is your lifeline. You will need to protect your access. Wash your area with soap and warm water every day. Check the area for signs of infection, such as heat or redness. When blood is flowing from your access and your reach is working well, you can feel the vibration on this area. If you cannot feel the vibration then tell your dialysis center.
Change what you eat and drink
If you are on hemodialysis, you may need to limit some food
* Sodium in foods and drinks.
* High Phosphorus Foods.
* The liquid you drink, including the liquid found in foods, stops in your body between hemodialysis treatments.
* Include proper amount of protein in your diet
* Choose foods with the right amount of potassium
* Take vitamins for people with kidney failure
* If you do not have a good appetite, then eat high calorie food.
Meet a dietitian to develop a meal plan that works for you.
You may feel better by eating the right foods when hemodialysis occurs. Talk to the dietitian at your dialysis center to find a hemodialysis meal plan that works for you.
How do I know if my hemodialysis is working?
You know how your hemodialysis treatment is working. Your energy levels may increase and you may feel better hungry. Hemodialysis reduces salt and fluid buildup, so you should also have shortness of breath and swelling.
To get the most out of your hemodialysis treatment, keep your ideal "dry weight". Your ideal dry weight is your weight when you do not have excess fluid in your body. If you are careful about the sodium in your diet and hemodialysis is working, then you should be able to reach your ideal dry weight at the end of every hemodialysis treatment. When hemodialysis treatments are working and you stay at your ideal dry weight, then your blood pressure should be well controlled.
In addition, blood tests can show how well your hemodialysis treatments are working. Once a month, whether you are at home or at dialysis center hemodialysis, your dialysis center will test your blood. Read more about hemodialysis dosage and adequacy.
What are the possible problems with hemodialysis?
Having problems with your vascular access is one of the most common problems.
* Infection
* There is poor blood flow or blockage from a blood clot or scar
These problems may prevent your treatment from working. To make it work properly you may need to do more procedures to change or improve your access.
A sudden change in your body's water and chemical balance during treatment can cause additional problems, such as
* muscle cramps.
* A sudden drop in blood pressure, called hypotension. Hypotension can make your stomach feel weak, dizzy or sick.
Your doctor may change your dialysis prescription to help avoid these problems. Longer and more frequent treatment of domestic hemodialysis is less likely than normal dialysis to cause muscle spasms or rapid changes in blood pressure.
You may lose blood if a needle comes out of an accident or a tube comes out of the dialyzer. To prevent blood loss, dialysis machines have a blood leak detector that sets off alarms. If this problem occurs in the clinic, a nurse or technician will be on hand to perform the work.
You may need a few months to adjust hemodialysis. Always report problems to your health care team, which can often quickly and easily treat side effects. You can avoid many side effects by following an eating plan with the advice of your dietician, limiting fluid intake and taking your medications as directed.
What if I'm on dialysis and I decide to stop?
If you are on dialysis and want to stop, you can still discuss further options with your doctor.
Author:
Dr. Anil Prasad Bhatt
Director – Nephrology | Fortis Hospital, Noida
Hemodialysis: All you need to know
Hemodialysis is a treatment for filtering waste and water from your blood, as your kidneys did when they were healthy. Hemodialysis helps to control important minerals such as potassium, sodium, and calcium in your blood and control blood pressure.
Hemodialysis can help you feel better and live longer, but it is not a treatment for kidney failure.
What happens during hemodialysis?
During hemodialysis, your blood goes through a filter, which is called a dialyzer outside your body. The dialyzer is sometimes called the "artificial kidney".
At the beginning of a hemodialysis treatment, a dialysis nurse or technician places two needles in your hand. Numb cream or spray may be used if the needle irritates you. Each needle is attached to a soft tube connected to a dialysis machine.
During hemodialysis, your blood is pumped through a filter, called a dialyzer.
The dialysis machine pumps blood through the filter and brings blood back to your body. During the procedure, the dialysis machine checks your blood pressure and controls how quickly
* Blood flows through the filter
* Fluids are released from your body
What happens to my blood when in the filter?
Blood enters one end of the filter and is forced into several, very thin, hollow fibers. As your blood passes through the hollow fibers, the dialysis solution passes in the opposite direction to the outside of the fibers. Waste products from your blood move to the dialysis solution. The filtered blood stays in hollow fibers and returns to your body.
In the filter, your blood flows inside hollow fibers that filter waste and excess salt and water.
Your nephrologist - a doctor specializing in kidney problems - will prescribe a dialysis prescription to meet your needs. The dialysis solution contains water and chemicals that are added to safely remove waste, excess salt, and fluid from your blood. Your doctor may adjust the balance of the chemicals in the solution if
* Your blood test shows that you have few or very few minerals in your blood, such as potassium or calcium
* You have problems like low blood pressure or muscle cramps during dialysis
Has the dialyzer done everything to get my kidneys at once?
No, hemodialysis can change part of your kidney function, but not all. Dialysis will help improve your energy level, and the changes you make to your diet can help you feel better. Limiting how much water and other fluids you drink through foods can help keep too much fluid from building up in your body between treatments. Medications during dialysis help you in maintaining your health.
Where can I get hemodialysis?
You can get treatment at a dialysis center or at home. Every place has its pros and cons.
Dialysis center
Most people go to a dialysis center for treatment. At the dialysis center, health care professionals are set up and help you connect with the dialysis machine. A team of health care workers will be available to assist you. You will continue to see your doctor. Other members of the team may include nurses, health care technicians, a dietitian and a social worker.
Set schedule
You will have a fixed time slot for your treatment, usually three times per week: Monday, Wednesday, and Friday; Or Tuesday, Thursday and Saturday. Each dialysis session lasts approximately 4 hours. When choosing a dialysis schedule, think about your work and child care or other caregiver duties.
Night option
Some dialysis centers offer nocturnal treatment. These treatments take place at a dialysis center 3 nights a week at bedtime, which takes longer. Now overnight dialysis treatment means
* Your days are free.
* You have less dietary changes.
* Your liquid allowance (how much liquid you can drink) is close to normal.
* You may have a better quality of life than the standard hemodialysis schedule. Long treatment sessions can ease your symptoms.
How can I get a dialysis center?
Seek the help of your doctor. Most major cities have more than one dialysis center to choose from. You can visit the centers to see which one of your requirements is most suitable. For example, you can ask about the use of laptops and cellphones as well as the rules of a center for visitors. You want the center to be close to your home to save travel time. If you live in a rural area, the nearest dialysis center may be away from your home. If you have a hard time coming to a dialysis center, you may want to consider home dialysis treatments such as home hemodialysis or peritoneal dialysis.
Home hemodialysis
Home hemodialysis allows you longer or more frequent dialysis, as do healthy kidneys - usually three to seven times per week, and with treatment sessions that last 2 to 10 hours. Machines for home use are small enough to sit on an end table.
If you want to do your treatment at home, you still consult your doctor once per month.
Flexible schedule
You can choose a schedule that fits your way of living. you can use
* Normal household hemodialysis - 3 to 5 hours three times a week or every other day
* Short daily hemodialysis - 5 to 7 days per week for 2 to 4 hours at a time
* Perform hemodialysis at night - three to six times per week at bedtime
Your doctor will decide how many treatments you need each week for daily or nightly home hemodialysis.
More dialysis filters your blood more thoroughly
Compared with a normal hemodialysis, daily or overnight household hemodialysis will give you
* Eat and drink more commonly
* Take low blood pressure medications
Healthy kidneys work 24 hours, 7 days a week. Getting more hemodialysis has the benefits of having a healthy kidney and lessens your chances for problems with a normal hemodialysis, such as
* Cramps by quickly removing too much fluid in painful muscles
* High blood pressure, which can cause a headache or, in rare cases, a stroke
* Low blood pressure, which can make you unconscious, make you feel sick in your stomach, or more likely to fall
* High phosphate levels, which can weaken bones and itch your skin
Better quality of life
You may feel tired for several hours after each treatment with normal hemodialysis. Those who have switched from normal hemodialysis to longer or persistent hemodialysis report feeling better with more energy, less nausea, and better sleep. They can also report better quality of life
How do I prepare for hemodialysis?
Dialysis is a complex treatment that takes time to understand. Because most people do not feel ill until shortly before starting dialysis, you will still feel good when your doctor talks to you about getting ready for dialysis. No one wants to get you started on dialysis before you need it, but preparing for dialysis takes time.
Take care of the blood vessels in your arms
It is important for you to protect your hand veins before starting dialysis. If you have kidney disease, health care providers should remind them to pour blood into the veins below your wrist and only IV lines; For example, ask them to use a vein on the back of their hand. If the vein of one arm is damaged by the IV line or by repeated blood drawing, it may not be used for vein dialysis.
Vascular Access Surgery
An important step before starting hemodialysis treatment is minor surgery to create vascular access. Your vascular access will be your lifeline, through which you will connect with the dialer. Dialysis transfers blood through the filter at a high rate. Blood flow is very strong. The machine extracts and returns about one point of blood from your body every minute. The access will be the place on your body where you insert needles to allow your blood to flow and return to your body at a high rate of dialysis by needle.
Three types of vascular access exist
* AV Fischula
* AV graft
* A catheter
Work closely with your nephrologist and vascular surgeon - a surgeon who works with blood vessels - to ensure that the vascular access is ready for use when you are ready for dialysis.
The surgeon connects a vein to a vein to make an AV fistula.
Avi fistula
The best type of long-term access is an AV facula. To make an AV fistula, a surgeon usually connects a vein to your hand. An artery is a blood vessel that carries blood away from your heart. A vein is a blood vessel that carries blood to your heart. When the surgeon connects an artery to a vein, the vein becomes wider and thicker, making it easier for the needles to give space for dialysis. The AV fistula also has a larger diameter that allows your blood to drain out and return quickly to your body. The goal is to allow high blood flow so that the greatest amount of blood can pass through the dialyzer.
The AV fistula is a blood vessel that is widened and strengthened by surgeons with needles that allow blood to exit and return to the dialysis machine.
AV fistula is considered the best option because it
* Provides the highest blood flow for dialysis
* Less likely to become infected or clot
* lasts longer
Most people can go home after outpatient surgery. And most operations are performed in local anesthesia.
AV grafts
If problems with your veins prevent you from having an AV fistula, you may need an AV graft instead. To make AV grafts, your surgeon uses a man-made tube to connect an artery to a vein. You can use AV grafts for dialysis immediately after surgery. However, you are more likely to have infections and blood clotting problems. Repeated blood clots can stop the flow of blood through the graft and make dialysis difficult or impossible.
Catheter for temporary access
If your kidney disease has progressed quickly, or you have not had vascular access before needing dialysis, you may need a venous catheter - a small, soft tube called a vein in your neck, chest, or leg. Is inserted in As temporary access. A nephrologist or an interventional radiologist - a doctor who uses medical imaging devices to perform the surgery - implants Venous catheters when you are in a hospital or in an outpatient clinic. You will receive local anesthesia and medication to keep you calm and relaxed during the procedure.
What changes do I need to make when I start hemodialysis?
You have to adjust your life to include your dialysis treatment sessions in your routine. If you have in-center dialysis, you may need to rest after each treatment. Adjusting for the effects of kidney failure and the time you spend on dialysis can be difficult. You may need to make changes in your work or home life by abandoning certain activities and responsibilities. It can be difficult for you and your family to accept these changes.
You have to change what you eat and drink. Your health care team can adjust the medicines you take.
Take care of your access
Your access is your lifeline. You will need to protect your access. Wash your area with soap and warm water every day. Check the area for signs of infection, such as heat or redness. When blood is flowing from your access and your reach is working well, you can feel the vibration on this area. If you cannot feel the vibration then tell your dialysis center.
Change what you eat and drink
If you are on hemodialysis, you may need to limit some food
* Sodium in foods and drinks.
* High Phosphorus Foods.
* The liquid you drink, including the liquid found in foods, stops in your body between hemodialysis treatments.
* Include proper amount of protein in your diet
* Choose foods with the right amount of potassium
* Take vitamins for people with kidney failure
* If you do not have a good appetite, then eat high calorie food.
Meet a dietitian to develop a meal plan that works for you.
You may feel better by eating the right foods when hemodialysis occurs. Talk to the dietitian at your dialysis center to find a hemodialysis meal plan that works for you.
How do I know if my hemodialysis is working?
You know how your hemodialysis treatment is working. Your energy levels may increase and you may feel better hungry. Hemodialysis reduces salt and fluid buildup, so you should also have shortness of breath and swelling.
To get the most out of your hemodialysis treatment, keep your ideal "dry weight". Your ideal dry weight is your weight when you do not have excess fluid in your body. If you are careful about the sodium in your diet and hemodialysis is working, then you should be able to reach your ideal dry weight at the end of every hemodialysis treatment. When hemodialysis treatments are working and you stay at your ideal dry weight, then your blood pressure should be well controlled.
In addition, blood tests can show how well your hemodialysis treatments are working. Once a month, whether you are at home or at dialysis center hemodialysis, your dialysis center will test your blood. Read more about hemodialysis dosage and adequacy.
What are the possible problems with hemodialysis?
Having problems with your vascular access is one of the most common problems.
* Infection
* There is poor blood flow or blockage from a blood clot or scar
These problems may prevent your treatment from working. To make it work properly you may need to do more procedures to change or improve your access.
A sudden change in your body's water and chemical balance during treatment can cause additional problems, such as
* muscle cramps.
* A sudden drop in blood pressure, called hypotension. Hypotension can make your stomach feel weak, dizzy or sick.
Your doctor may change your dialysis prescription to help avoid these problems. Longer and more frequent treatment of domestic hemodialysis is less likely than normal dialysis to cause muscle spasms or rapid changes in blood pressure.
You may lose blood if a needle comes out of an accident or a tube comes out of the dialyzer. To prevent blood loss, dialysis machines have a blood leak detector that sets off alarms. If this problem occurs in the clinic, a nurse or technician will be on hand to perform the work.
You may need a few months to adjust hemodialysis. Always report problems to your health care team, which can often quickly and easily treat side effects. You can avoid many side effects by following an eating plan with the advice of your dietician, limiting fluid intake and taking your medications as directed.
What if I'm on dialysis and I decide to stop?
If you are on dialysis and want to stop, you can still discuss further options with your doctor.
Author:
Dr. Anil Prasad Bhatt
Director – Nephrology | Fortis Hospital, Noida