A Comprehensive Guide About Liver Cirrhosis
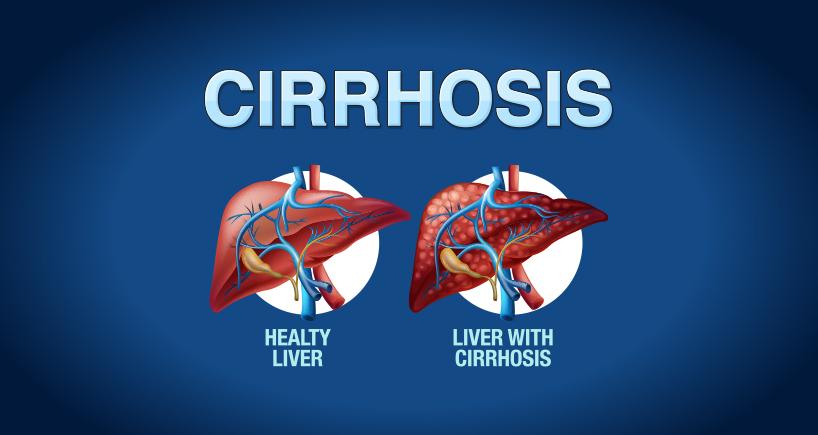
Liver cirrhosis is a serious condition that affects the liver, the largest organ in the body. The liver performs many vital functions, such as filtering toxins, producing bile, and making blood proteins. However, when the liver is damaged by chronic inflammation, scar tissue replaces healthy tissue and impairs the liver’s ability to function properly. This is called liver cirrhosis.
In this blog post, we will explain the symptoms, causes, stages, and treatment options for liver cirrhosis. We hope this information will help you understand this condition better and take steps to prevent or manage it.
What are the symptoms of liver cirrhosis?
Liver cirrhosis often has no symptoms in the early stages, as the liver can still compensate for the damage. However, as the disease progresses, the symptoms become more noticeable and severe. Some of the common symptoms of liver cirrhosis are:
- Fatigue and weakness
- Loss of appetite and weight loss
- Nausea and vomiting
- Upper abdominal pain
- Swelling of the legs, feet, or ankles (edema)
- Itchy skin
- Yellow discoloration of the skin and eyes (jaundice)
- Fluid accumulation in the abdomen (ascites)
- Spider-like blood vessels on the skin (spider angiomas)
- Redness of the palms of the hands
- Pale or brittle fingernails
- For women, absence or irregularity of periods not related to menopause
- For men, loss of sex drive, testicular shrinkage, or breast enlargement (gynecomastia)
- Confusion, drowsiness, or slurred speech (hepatic encephalopathy)
- Easy bruising or bleeding
- Increased risk of infections
If you notice any of these symptoms, it is important to consult or book an appointment with a medical professional immediate diagnosis or treatment.
What are the causes of liver cirrhosis?
Liver cirrhosis can be caused by a variety of factors that damage the liver over a long period of time. Several factors that contribute to the cause of liver cirrhosis are:
- Chronic alcohol consumption: Excessive alcohol consumption can cause inflammation and scarring of the liver, leading to cirrhosis. Alcohol is one of the leading causes of liver cirrhosis worldwide.
- Chronic viral hepatitis: Hepatitis B, C, and D, are viral infections that can cause inflammation and damage to the liver. If left untreated, they can lead to chronic liver disease and cirrhosis. Hepatitis B and C are the most common causes of liver cirrhosis in India.
- Non-alcoholic fatty liver disease (NAFLD): This is a condition in which fat accumulates in the liver, causing inflammation and scarring. It is often associated with obesity, diabetes, high cholesterol, and metabolic syndrome. NAFLD is becoming more prevalent as a cause of liver cirrhosis due to the increasing rates of these risk factors.
- Other causes: There are many other less common causes of liver cirrhosis, such as:
- Hemochromatosis: A genetic disorder that causes excess iron to build up in the body, damaging the liver and other organs.
- Wilson’s disease: A genetic disorder that causes excess copper to accumulate in the body, damaging the liver and other organs.
- Cystic fibrosis: A genetic disorder that affects the lungs and digestive system, causing thick mucus to block the bile ducts and damage the liver.
- Biliary atresia: A congenital defect that causes the bile ducts to be poorly formed or absent, preventing bile from flowing out of the liver and causing damage.
- Autoimmune hepatitis: A condition in which the immune system attacks the liver, causing inflammation and scarring.
- Primary biliary cholangitis: A condition in which the immune system attacks the bile ducts, causing inflammation and scarring.
- Primary sclerosing cholangitis: A condition in which the bile ducts become hardened and scarred, obstructing the flow of bile and causing damage to the liver.
What are the stages of liver cirrhosis?
Liver cirrhosis is a progressive condition that worsens as more scar tissue develops and replaces healthy tissue. Liver cirrhosis can be classified into four stages, depending on the extent of liver damage and the presence of complications. These stages are:
- Stage 1: Compensated cirrhosis. This is the earliest stage of cirrhosis, in which the liver can still perform its functions despite the damage. There are no symptoms or complications at this stage. Effective treatment can either prevent or slow down the rate of progression of the disease.
- Stage 2: Compensated cirrhosis with varices. This is the stage in which the scar tissue blocks the blood flow through the liver, causing high blood pressure in the portal vein (portal hypertension). This leads to the formation of enlarged veins (varices) in the oesophagus, stomach, or intestines, which can rupture and bleed. Bleeding varices are a serious complication that can be life-threatening. Treatment can prevent or stop the bleeding and reduce the portal hypertension.
- Stage 3: Decompensated cirrhosis with ascites. This is the stage in which the liver function declines significantly, causing fluid to accumulate in the abdomen (ascites). Ascites can cause abdominal discomfort, breathing difficulties, infection, and kidney failure. Treatment can drain the fluid and prevent or treat the complications.
- Stage 4: Decompensated cirrhosis with hepatic encephalopathy. This is the final stage of cirrhosis, in which the liver function deteriorates to the point that it can no longer remove toxins from the blood. This causes the toxins to build up in the brain, causing confusion, drowsiness, or coma (hepatic encephalopathy). Hepatic encephalopathy is a severe complication that can be fatal. Treatment can reduce the toxins and improve the mental state.
Treatment options for liver cirrhosis
The treatment of liver cirrhosis depends on the cause, the stage, and the complications of the condition. The main goals of treatment are to slow down the progression of liver damage, relieve the symptoms, and prevent or treat the complications. Some of the common treatment options are:
- Medications: Depending on the cause of liver cirrhosis, medications may be prescribed to treat the underlying condition, such as antiviral drugs for hepatitis, corticosteroids for autoimmune hepatitis, or chelating agents for hemochromatosis. Medications may also be used to treat the symptoms and complications of liver cirrhosis, such as diuretics for edema and ascites, lactulose for hepatic encephalopathy, or beta blockers for portal hypertension.
- Lifestyle changes: Lifestyle changes are essential to prevent further liver damage and improve liver function. These include avoiding alcohol and drugs, eating a healthy and balanced diet, limiting salt and fluid intake, exercising regularly, and maintaining a healthy weight. Smoking cessation, vaccination, and safe sex practices are also important to prevent infections and complications.
- Procedures: In some cases, procedures may be performed to treat the complications of liver cirrhosis, such as endoscopic variceal ligation (EVL) or trans jugular intrahepatic portosystemic shunt (TIPS) for bleeding varices, paracentesis or peritoneovenous shunt for ascites, or liver transplant for liver failure.
- Liver transplant: Liver transplant is the only definitive treatment for liver cirrhosis, as it replaces the damaged liver with a healthy one from a donor. However, liver transplant is not suitable for everyone, as there are strict criteria and risks involved. Moreover, there is a shortage of donor organs, and the waiting time can be long. Therefore, liver transplant is usually reserved for patients with end-stage liver cirrhosis who have a poor prognosis and no other treatment options.
Prevention of liver cirrhosis
The best way to prevent or delay liver cirrhosis is to avoid or treat the factors that can cause liver damage. Some of the preventive measures that you can take are:
- Limit or avoid alcohol consumption, as alcohol is one of the leading causes of liver cirrhosis.
- Get vaccinated against hepatitis A and B, as these are viral infections that can cause liver inflammation and scarring. There is no vaccine for hepatitis C, but you can prevent it by avoiding exposure to infected blood or body fluids.
- Practise good hygiene and avoid sharing needles, razors, toothbrushes, or other personal items that may carry blood or body fluids.
- Have a balanced and nutritious diet, as malnutrition can worsen liver damage and cause complications. Avoid foods that are high in fat, salt, or sugar, and limit your intake of processed or fried foods. Include foods that are rich in protein, fibre, vitamins, and minerals, such as fruits, vegetables, whole grains, lean meats, fish, eggs, nuts, and seeds.
- Drink plenty of water, as dehydration can affect the liver function and increase the risk of infections. Aim for at least eight glasses of water a day, or more if you have fluid retention or ascites.
- Exercise regularly, as physical activity can improve the blood circulation, metabolism, and immune system, and prevent obesity, diabetes, and other risk factors for liver cirrhosis.
- Quit smoking, as tobacco can damage the liver and increase the risk of liver cancer. Smoking can also worsen the symptoms and complications of liver cirrhosis, such as bleeding, infection, or hepatic encephalopathy.
- Manage your stress, as stress can affect the liver function and cause inflammation and scarring. Stress can also trigger or worsen the symptoms and complications of liver cirrhosis, such as fatigue, nausea, or depression. Find healthy ways to cope with stress, such as meditation, yoga, breathing exercises, hobbies, or counselling.
Liver cirrhosis is a serious condition that requires medical attention and lifestyle changes. By following these tips, you can prevent or delay liver cirrhosis and improve your health and well-being. If you have any questions or concerns about liver cirrhosis, please contact or book an appointment today at Fortis Hospital.